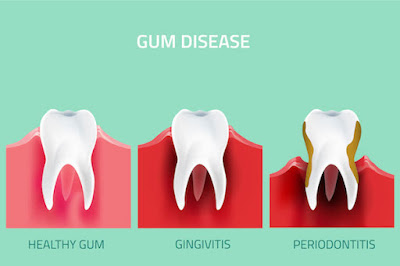
DIFFRENCE BETWEEN GINGIVITIS AND PERODONTITIS
Gingivitis and Periodontitis, two words you do not want coming out of your dentist’s mouth at your next check-up. Let's pause and take a deep breath here. Their unpleasant names alone are enough to scare anyone. But what is the difference between these two very serious dental diseases? What is gingivitis? Gingivitis is gum inflammation and, when left untreated, can progress to more serious stages of periodontal disease, such as periodontitis. Plaque accumulates in the areas between the teeth, which inflame the gums and they start to bleed easily. Clear signs of gingivitis are red, swollen gums or gums that bleed easily when you brush your teeth. Even though gums are irritated, gum recession does not occur until later stages of periodontal disease. Gingivitis is a warning sign from the teeth and gums that you must be more proactive about your oral hygiene routine. There is also no irreversible bone damages during gingivitis. This makes it important for those diagnosed with gingivitis to visit our office at 32 PEARLS for a routine dental cleaning that can remove this plaque and restore your oral health. Gingivitis usually precedes periodontitis, which is the leading cause of tooth loss in adults. Not all gingivitis progresses to periodontitis. The major difference between the two is that gingivitis is reversible, while periodontitis is not. If left unattended, gingivitis can advance to periodontitis. Gingivitis is a clear warning sign from our teeth and gums that we must be more proactive about our oral and overall health. Good oral hygiene habits like brushing twice a day, regular dental check-ups, daily flossing and use of mouthwash can help, prevent and reverse gingivitis. What causes gingivitis? There are many factors that may increase your risk of developing gingivitis, including: Smoking: In addition to being one of the biggest risk factors for gum disease, smoking also lowers the chances that treatment will be effective. Poor oral hygiene: Not brushing or flossing regularly can lead to the onset of gingivitis. Hormonal changes: Hormone changes, like those that occur during puberty, pregnancy, or menopause can lead to an increased chance of sensitivity and inflammation in your gums. Taking care of your teeth and gums will help to reduce this risk. Poor diet: Poor nutrition deprives your body of important vitamins and minerals. This makes it more difficult to fight off infections, such as gum disease. Chronic disease: Diabetes, HIV, or cancer are all examples of medical conditions that make you more susceptible to fighting infection. Our periodontal specialists can help you establish an effective oral hygiene routine that will reduce your risk of developing gum disease.
What is It is the Period ontitis ? Inflammation of the Surrounding Hard Tissues of the Teeth . When periodontitis develops, the inner layer of the gum and bone pull away from the teeth and form pockets. These small spaces between teeth and gums collect debris and can becom e infected. The body’s immune system fights the bacteria as the plaque spreads and grows below the gum line. Our immune system’s fight to save our gums is not an easy one. The toxins and poisons produced by the bacteria in plaque teams with our body’s “go od” enzymes involved in fighting infections to weaken and break down bone and collective tissue that hold teeth in place. The pockets deepen and even more gum tissue and bone are destroyed. At this advanced stage of gum disease teeth are no longer anchore Tooth loss often follows. e your d in place. They become loose. Symptoms of periodontitis include continued red, swollen or bleeding gums, pain when chewing, poor tooth alignment, receding gums and clear pockets between teeth and gums. At this point, you must se periodontist as soon as possible. How can you tell if you have gingivitis or periodontitis? Here are some tips on how to tell the difference: Age : Usually periodontitis is rare in teenagers, but they can develop gingivitis.
How can you tell if you have gingivitis or periodontitis? Here are some tips on how to tell the difference: Age : Usually periodontitis is rare in teenagers, but they can develop gingivitis.
Pain: Pain when chewing can be a sign that your periodontal disease has progressed from gingivitis to periodontitis. Tooth Condition: If you have gingivitis, your teeth should be firmly in place, although your gums may be irritated, red and swollen. If a tooth or teeth are loose, it is more likely you have periodontitis. Breath: If your gingivitis has progressed to periodontitis, you may notice that you have persistent unpleasant breath due to the presence of excess bacteria in your mouth. Again, if you are experiencing symptoms of gum disease, it is imperative to call your dentist ASAP. Your dentist will examine your teeth and confirm the diagnosis. If caught early, periodontitis can be kept in check with a thorough dental cleaning and a strong at-home oral care routine. Remember, a gingivitis or early periodontitis diagnosis is not a death sentence for your teeth, but we must take it as a personal call to action to save our teeth. For the best long-term difference between gingivitis and periodontitis is ensuring gingivitis doesn’t become gum disease. We examine you for gum health at every 6-month check-up. If you have been experiencing any symptoms like bad breath, bleeding or tender gums, please let us know. What are different Periodontal disease treatment approaches? The periodontal disease treatment that will work best for you is determined by the severity of your gum disease. Treating gum disease as early as possible minimizes damage and reduces the chances of tooth loss. Some common periodontal treatments that we use include: Dental cleaning: During a routine dental cleaning, we remove all plaque and tartar above and below the gum line. If we suspect any gum disease, we will recommend more frequent dental cleanings. Scaling and root planing: For gum disease cases found early, scaling and root planing is effective. Scaling and root planing is a deep-cleaning and nonsurgical procedure done while the patient is under local anaesthesia. Plaque and tartar are both scraped away from above and below the gum line. Rough spots on the tooth root are made smooth with planing. By smoothing these rough spots, we remove bacteria and provide a clean surface for your gums to properly reattach. Flap surgery/pocket reduction surgery: For more advanced stages of periodontal disease, such as periodontitis, surgery may be necessary. The gums are lifted back and any tartar is removed. In some cases, irregular surfaces of the damaged bone are smoothed where any disease-causing bacteria may be found. Your gums are then placed so that they fit snugly around your teeth. This will reduce the space between the gum and tooth. Bone grafts: This uses fragments of your own bone, donated bone, or even synthetic bone to replace any bone destroyed by gum disease. This procedure promotes regrowth of bone, which helps make your teeth more stable. Soft tissue grafts can also be used to reinforce thin gums or even to fill in places where gum recession has occurred. LANAP laser gum surgery: Our periodontal specialists use this surgery instead of traditional surgery
because it is less painful and reduces sensitivity post stop gum disease before it starts .
to know more about your gums and teeth click on link and read more.